You note the shown skin disorder during a general medical evaluation. You explain to the patient they are at risk for the development of:
A) Alzheimer's disease
B) tuberculosis
C) diabetes mellitus
D) Grave's disease
E) melanoma
The answer is C. (Diabetes mellitus)
Although the majority of cases of acanthosis nigricans are benign and associated with obesity, the disease can represent the onset of malignancy as well as a variety of conditions related to insulin resistance.
Acanthosis nigricans has been reported in association with a number of malignancies, particular gastrointestinal cancers (e.g., gastric, hepatocellular) and lung cancer. The suspicion for malignancy increases in patients with extensive or rapidly progressive lesions, when there is mucous membrane involvement, or when there is prominent sole and palm disease.
The common finding in all non-malignancy associated cases of acanthosis nigricans is insulin resistance. This explains the relationship between this skin disorder and diseases such as diabetes mellitus, Cushing's syndrome, and hypothyroidism (most likely due to weight gain and subsequent insulin resistance), and with obesity.
Tuesday, 23 August 2011
Photos of Melanosis coli "Pseudomelanosis coli"
Melanosis coli, also pseudomelanosis coli, is a disorder of pigmentation of the wall of the colon, often identified at the time of colonoscopy.
The most common cause of melanosis coli is the extended use of laxatives, this darkening of the colonic mucosa caused by the accumulation of lipofuscin particles within the macrophages of the lamina propria of the colonic mucosa as a result of long term exposure to anthraquinone-containing laxatives as Senna and other plant glycosides. However, other causes are identified, including an increase in colonic epithelial apoptosis.
- Melanosis coli is a misnomer, as the pigmentation is due to lipofuscin-laden macrophages - not melanin pigment. Pseudomelanosis coli is a more appropriate descriptor, but not in common usage.
The differential diagnosis of brown pigmentation of the colon is:
* Pseudomelanosis coli.
* Hemosiderin-laden macrophages (old haemorrhage).
* Melanin (rare).
The most common cause of melanosis coli is the extended use of laxatives, this darkening of the colonic mucosa caused by the accumulation of lipofuscin particles within the macrophages of the lamina propria of the colonic mucosa as a result of long term exposure to anthraquinone-containing laxatives as Senna and other plant glycosides. However, other causes are identified, including an increase in colonic epithelial apoptosis.
This is the photograph of the colon, and there is an extremely dark appearance to the wall of the colon. This is seen in patients who have taken laxatives over many years and the pigment from the laxative gets deposited in the wall of the bowel giving an extremely dark appearance to it. This is a benign condition, not cancerous, and does not become cancerous, but often it is quite obvious.
- Melanosis coli is a misnomer, as the pigmentation is due to lipofuscin-laden macrophages - not melanin pigment. Pseudomelanosis coli is a more appropriate descriptor, but not in common usage.
The differential diagnosis of brown pigmentation of the colon is:
* Pseudomelanosis coli.
* Hemosiderin-laden macrophages (old haemorrhage).
* Melanin (rare).
Saturday, 20 August 2011
Friday, 19 August 2011
Decompression sickness "divers' disease"
A 55-year-old male diver begins complaining of back pain and urinary retention 1 h after a dive. What is the MOST likely diagnosis?
Decompression sickness (DCS),also known as divers' disease, the bends or caisson disease, is caused by formation of gas bubbles in tissues after ascent from a dive and results in vascular occlusion, usually in the venous circulation. DCS may have cutaneous manifestations including rash and pruritus. It classically causes joint and back pain and may be associated with neurologic symptoms secondary to spinal cord involvement.
Patients with neurologic or other severe forms of DCS should be referred for hyperbaric oxygen therapy. Nitrogen narcosis is due to the anesthetic effects of breathing nitrogen at high partial pressures and causes divers to become altered on deep dives.
- (A)Barotrauma to the bladder
- (B)Lumbar strain
- (C)Neurotoxin from a marine envenomation
- (D)Nitrogen narcosis
- (E)Decompression sickness
The answer is E.
Barotrauma is the most common affliction of divers and usually affects the ears, sinuses, lungs, and, rarely, the gastrointestinal tract. The bladder is not involved.Decompression sickness (DCS),also known as divers' disease, the bends or caisson disease, is caused by formation of gas bubbles in tissues after ascent from a dive and results in vascular occlusion, usually in the venous circulation. DCS may have cutaneous manifestations including rash and pruritus. It classically causes joint and back pain and may be associated with neurologic symptoms secondary to spinal cord involvement.
Patients with neurologic or other severe forms of DCS should be referred for hyperbaric oxygen therapy. Nitrogen narcosis is due to the anesthetic effects of breathing nitrogen at high partial pressures and causes divers to become altered on deep dives.
Superior vena cava syndrome
A 72-year-old man who was overweight and had a history of hypertension and heavy smoking presented with a swollen neck. He had no dysphagia. He reported that he had experienced increased snoring and daytime sleepiness during the previous 3 weeks.
An otolaryngologic examination was unremarkable except for an unusually narrow upper airway. On inspection, the patient's hands were swollen and showed signs of pitting edema (Figure 1A). Inflammatory parameters and complete blood count were normal.
Contrast-enhanced computed tomography scans of the neck and chest revealed an enlarged retropharyngeal space (Figure 1B) and a mass compressing the superior vena cava (Figure 1C). A transthoracic needle biopsy showed a non–small-cell carcinoma. Radiotherapy resulted in clinical improvement and a rapid reduction in compression of the superior vena cava.
The exact incidence of superior vena cava syndrome remains unknown, It has mainly malignant causes.
Nonmalignant causes can include aneurysm of the aorta, thromboses after implanted intravascular catheters or fibrosing mediastinitis.
Classically, compression of the superior vena cava leads to visible swelling and venous distension in the face, neck, chest and upper limbs. Other symptoms of varying severity can occur, from cough, hoarseness and dyspnea to headache, confusion and visual symptoms. In patients who are overweight, swelling of the neck may go unnoticed, and signs such as obstructive sleep apnea or edema of the upper limb may point to the diagnosis.
An otolaryngologic examination was unremarkable except for an unusually narrow upper airway. On inspection, the patient's hands were swollen and showed signs of pitting edema (Figure 1A). Inflammatory parameters and complete blood count were normal.
Contrast-enhanced computed tomography scans of the neck and chest revealed an enlarged retropharyngeal space (Figure 1B) and a mass compressing the superior vena cava (Figure 1C). A transthoracic needle biopsy showed a non–small-cell carcinoma. Radiotherapy resulted in clinical improvement and a rapid reduction in compression of the superior vena cava.
The exact incidence of superior vena cava syndrome remains unknown, It has mainly malignant causes.
Nonmalignant causes can include aneurysm of the aorta, thromboses after implanted intravascular catheters or fibrosing mediastinitis.
Classically, compression of the superior vena cava leads to visible swelling and venous distension in the face, neck, chest and upper limbs. Other symptoms of varying severity can occur, from cough, hoarseness and dyspnea to headache, confusion and visual symptoms. In patients who are overweight, swelling of the neck may go unnoticed, and signs such as obstructive sleep apnea or edema of the upper limb may point to the diagnosis.
Monday, 15 August 2011
Characteristic shape of Molluscum contagiosum infection
A 4-year-old preschooler presents with the skin lesions shown here. The area affected is just below the chin on the child's right side. The lesions have been present over the last month, and the child has reported no symptoms associated with them. The most likely diagnosis is
The lesions are dome-shaped, waxy, or pearly-white papules with a central white core and are 1 to 3 mm in diameter. Frequently, groups of lesions are found. The lesions may resolve spontaneously. Treatment involves removal with a sharp needle or curette, application of liquid nitrogen, antiwart preparations, electrodessication and curettage, or trichloroacetic peels for extensive areas. Typically, infants or young preschool-age children should not be treated aggressively.
- A) varicella
- B) herpes zoster
- C) Rhus dermatitis
- D) molluscum contagiosum
- E) scabies
The answer is D. (Molluscum contagiosum)
Molluscum contagiosum is a common, superficial viral infection of the skin that typically occurs in infants and preschoolers. The incidence decreases after the age of 6 to 7 years. The condition can be spread via sexual contact in young adults.The lesions are dome-shaped, waxy, or pearly-white papules with a central white core and are 1 to 3 mm in diameter. Frequently, groups of lesions are found. The lesions may resolve spontaneously. Treatment involves removal with a sharp needle or curette, application of liquid nitrogen, antiwart preparations, electrodessication and curettage, or trichloroacetic peels for extensive areas. Typically, infants or young preschool-age children should not be treated aggressively.
Typical flesh-colored, dome-shaped and pearly lesions
Friday, 12 August 2011
Thursday, 11 August 2011
Synthesis and metabolism of vitamin D in the regulation of calcium, phosphorus, and bone metabolism.
Click for photo enlargement
During exposure to solar UVB radiation, 7-dehydrocholesterol in the skin is converted to previtamin D3, which is immediately converted to vitamin D3 in a heat-dependent process. Excessive exposure to sunlight degrades previtamin D3 and vitamin D3 into inactive photoproducts. Vitamin D2 and vitamin D3 from dietary sources are incorporated into chylomicrons and transported by the lymphatic system into the venous circulation. Vitamin D (hereafter, “D” represents D2 or D3) made in the skin or ingested in the diet can be stored in and then released from fat cells.Vitamin D in the circulation is bound to the vitamin D–binding protein, which transports it to the liver, where vitamin D is converted by vitamin D-25-hydroxylase to 25(OH)D. This is the major circulating form of vitamin D that is used by clinicians to determine vitamin D status. (Although most laboratories report the normal range to be 20 to 100 ng/mL [50 to 250 nmol/L], the preferred range is 30 to 60 ng/mL [75 to 150 nmol/L].) This form of vitamin D is biologically inactive and must be converted in the kidneys by 25-hydroxyvitamin D-1α-hydroxylase (1-OHase) to the biologically active form 1,25(OH)2D.
Serum phosphorus, calcium, fibroblast growth factor 23 (FGF-23), and other factors can either increase (+) or decrease (−) the renal production of 1,25(OH)2D. 1,25(OH)2D decreases its own synthesis through negative feedback and decreases the synthesis and secretion of PTH by the parathyroid glands. 1,25(OH)2D increases the expression of 25-hydroxyvitamin D-24-hydroxylase (24-OHase) to catabolize 1,25(OH)2D to the water-solubl biologically inactive calcitroic acid, which is excreted in the bile.
1,25(OH)2D enhances intestinal calcium absorption in the small intestine by interacting with the vitamin D receptor–retinoic acid x-receptor complex (VDR-RXR) to enhance the expression of the epithelial calcium channel (transient receptor potential cation channel, subfamily V, member 6 [TRPV6]) and calbindin 9K, a calcium-binding protein (CaBP). 1,25(OH)2D is recognized by its receptor in osteoblasts, causing an increase in the expression of the receptor activator of RANKL.
RANK, the receptor for RANKL on preosteoclasts, binds RANKL, which induces preosteoclasts to become mature osteoclasts. Mature osteoclasts remove calcium and phosphorus from the bone, maintaining calcium and phosphorus levels in the blood. Adequate Ca2+ and phosphorus (HPO42−) levels promote the mineralization of the skeleton.
Tuesday, 9 August 2011
8 clinical criteria predict management in an ICU
Which of the following would indicate the patient must be monitored in an intensive care unit setting following an overdose?
Answer and Discussion
The answer is E.
The presence of any of eight clinical criteria predict a complicated hospital course that could be best managed in an ICU:
1- PaCO2 >45 mmHg
2- A need for emergency intubation
3- The presence of postingestion seizures
4- Unresponsiveness to verbal stimuli
5- A non-sinus cardiac rhythm
6- Second- or third-degree atrioventricular block
7- Systolic blood pressure <80 mmHg
8- QRS duration ≥ 0.12 seconds
- A) PaCO2 >45 mmHg
- B) Seizures
- C) QRS duration ≥ 0.12 seconds
- D) Second- or third-degree atrioventricular block
- E) All of the above
Answer and Discussion
The answer is E.
The presence of any of eight clinical criteria predict a complicated hospital course that could be best managed in an ICU:
1- PaCO2 >45 mmHg
2- A need for emergency intubation
3- The presence of postingestion seizures
4- Unresponsiveness to verbal stimuli
5- A non-sinus cardiac rhythm
6- Second- or third-degree atrioventricular block
7- Systolic blood pressure <80 mmHg
8- QRS duration ≥ 0.12 seconds
Friday, 5 August 2011
Description of Hallux Malleus "hammer toe"
-Hallux for the big toe
-Malleus for a hammer
Hallux malleus is a deformity of the great toe. This deformity can be very stiff or flexible. The joint in the great toe becomes contracted in a flexed or downward position.
This deformity usually occurs due to an imbalance of the tendons that insert on the top and the bottom of the great toe. When the tendon on the bottom of the toe (the tendon that causes the toe to flex down) over powers the tendon that causes the toe to bend up, this deformity occurs.
Usually patients will develop a callus and even an ulcer on the tip of the great toe. This deformity is often seen in conjunction with hammer toes. High arched feet are typically the most affected by this deformity.
This deformity is treat initially with padding techniques to prevent sores from developing at the tip of the toe. Custom, soft, accommodative orthoses are sometimes prescribed for the patient to provide cushioning and also to prevent worsening of the deformity.
If conservative treatment fails, surgery is indicated. Surgery usually consists of performing a bone fusion of the 2 bones in the great toe. This can be done with screws, staples, or wire fixation.
-Malleus for a hammer
Hallux malleus is a deformity of the great toe. This deformity can be very stiff or flexible. The joint in the great toe becomes contracted in a flexed or downward position.
This deformity usually occurs due to an imbalance of the tendons that insert on the top and the bottom of the great toe. When the tendon on the bottom of the toe (the tendon that causes the toe to flex down) over powers the tendon that causes the toe to bend up, this deformity occurs.
Usually patients will develop a callus and even an ulcer on the tip of the great toe. This deformity is often seen in conjunction with hammer toes. High arched feet are typically the most affected by this deformity.
This deformity is treat initially with padding techniques to prevent sores from developing at the tip of the toe. Custom, soft, accommodative orthoses are sometimes prescribed for the patient to provide cushioning and also to prevent worsening of the deformity.
If conservative treatment fails, surgery is indicated. Surgery usually consists of performing a bone fusion of the 2 bones in the great toe. This can be done with screws, staples, or wire fixation.
Thursday, 4 August 2011
About Retinal Detachments
Which of the following statements is TRUE regarding acute traumatic retinal detachments?
Detachments begin as small tears in the ora serrata (called dialysis), most frequently affecting the inferotemporal quadrant, followed by the superonasal quadrant. Because most detachments are very peripherally situated on the retina, standard fundoscopy is typically inadequate for visualization. Although a number of techniques have been developed to correct the detachment, visual outcome remains largely determined by the degree of macular involvement.
- (A) Most detachments can be visualized on standard fundoscopy
- (B) Eighty percent of detachments occur within 24 h of the traumatic event
- (C) Most detachments originate in the inferotemporal quadrant
- (D) Visual outcome depends on the extent of involvement of the optic disc
- (E) Sudden onset of pain is a prominent feature
The answer is C.
The typical retinal detachment is heralded by painless flashes of light, floaters, and a shade across the visual field. Interestingly, most detachments follow a latent period, up to 8 months posttrauma in 50 percent of cases.Detachments begin as small tears in the ora serrata (called dialysis), most frequently affecting the inferotemporal quadrant, followed by the superonasal quadrant. Because most detachments are very peripherally situated on the retina, standard fundoscopy is typically inadequate for visualization. Although a number of techniques have been developed to correct the detachment, visual outcome remains largely determined by the degree of macular involvement.
Wednesday, 3 August 2011
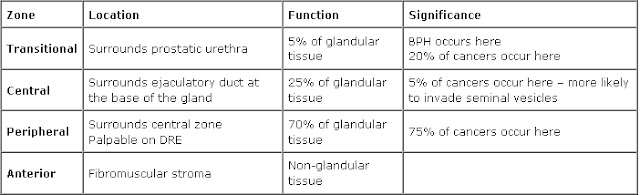
Prostate diseases in relation to Prostate zones
Most cancer lesions occur in the peripheral zone of the gland, fewer occur in the transition zone and almost none arise in the central zone. Most benign prostate hyperplasia (BPH) lesions develop in the transition zone, which might enlarge considerably beyond what is shown.
The inflammation found in the transition zone is associated with BPH nodules and atrophy, and the latter is often present in and around the BPH nodules. Acute inflammation can be prominent in both the peripheral and transition zones, but is quite variable.
The inflammation in the peripheral zone occurs in association with atrophy in most cases.
Although carcinoma might involve the central zone, small carcinoma lesions are virtually never found here in isolation, strongly suggesting that prostatic intraepithelial neoplasia (PIN) lesions do not readily progress to carcinoma in this zone. Both small and large carcinomas in the peripheral zone are often found in association with high-grade PIN, whereas carcinoma in the transition zone tends to be of lower grade and is more often associated with atypical adenomatous hyperplasia or adenosis, and less often associated with high-grade PIN. The various patterns of prostate atrophy, some of which frequently merge directly with PIN and at times with small carcinoma lesions, are also much more prevalent in the peripheral zone, with fewer occurring in the transition zone and very few occurring in the central zone.
The inflammation found in the transition zone is associated with BPH nodules and atrophy, and the latter is often present in and around the BPH nodules. Acute inflammation can be prominent in both the peripheral and transition zones, but is quite variable.
The inflammation in the peripheral zone occurs in association with atrophy in most cases.
Although carcinoma might involve the central zone, small carcinoma lesions are virtually never found here in isolation, strongly suggesting that prostatic intraepithelial neoplasia (PIN) lesions do not readily progress to carcinoma in this zone. Both small and large carcinomas in the peripheral zone are often found in association with high-grade PIN, whereas carcinoma in the transition zone tends to be of lower grade and is more often associated with atypical adenomatous hyperplasia or adenosis, and less often associated with high-grade PIN. The various patterns of prostate atrophy, some of which frequently merge directly with PIN and at times with small carcinoma lesions, are also much more prevalent in the peripheral zone, with fewer occurring in the transition zone and very few occurring in the central zone.
Subscribe to:
Posts (Atom)