Friday, 31 December 2010
Cardiac Pacemaker
It is represents External Energy Sources Used To Stimulate The Heart Primarily In Patients With Symptomatic Heart Blocks And Bradyarrhythmias.
Indication :
* Selection Of The Appropriate Pacemaker And Pacing Mode Depends On The Clinical Condition And The Type Of Bradyarrhythmia Being Treated* Temporary Pacing :
- For Symptomatic Bradicardia Due To Temporary Condition, Or As A Bridge To Permanent Pacer Placement
- Symptomatic Bradycardia Due To : SA Nodal Dysfunction, Irreversible 2nd Or 3rd Degree AV Block
- Recurrent Syncope Due To Carotid Sinus Hypersensitivity
- Chronotropic Incompetence Is Present
- An Increase In Heart Rate Is Required To Enchance Physiologic Performance
Happy Holidays from Stanford Hospital & Clinics 2010
Stanford Hospital & Clinics asked its employees what they are thankful for this holiday season, here are their answers.
Stanford Hospital & Clinics wishes everyone a very happy hoiday season and a happy New Year!
Stanford Hospital & Clinics wishes everyone a very happy hoiday season and a happy New Year!
Ramsay Hunt Syndrome(clinical)
CAUSES:
Classic Ramsay Hunt syndrome is ascribed to infection of the geniculate ganglion by herpesvirus 3 (varicella-zoster virus [VZV]).

HISTORY:
*Patients usually present with paroxysmal pain deep within the ear. The pain often radiates outward into the pinna of the ear and may be associated with a more constant, diffuse, and dull background pain.
*The onset of pain usually precedes the rash by several hours and even days.
*Classic Ramsay Hunt syndrome can be associated with the following:
-Vesicular rash of the ear or mouth (as many as 83% of cases),The rash might precede the onset of facial paresis/palsy.
-Ipsilateral lower motor neuron facial paresis/palsy (CN VII)
-Vertigo and ipsilateral hearing loss (CN VII)
-Tinnitus,Otalgia,Headaches,DysarthriaGait,ataxia.
-Fever,Cervical adenopathy.
*Facial weakness usually reaches maximum severity by one week after the onset of symptoms.
*Other cranial neuropathies might be present and may involve cranial nerves (CNs) VIII, IX, X, V, and VI.
*Ipsilateral hearing loss has been reported in as many as 50% of cases.
*Blisters of the skin of the ear canal, auricle, or both may become secondarily infected, causing cellulitis.
EXAMINATION:
.The primary physical findings in classic Ramsay Hunt syndrome include peripheral facial nerve paresis with associated rash or herpetic blisters in the distribution of the nervus intermedius.
.The location of the accompanying rash varies from patient to patient, as does the area innervated by the nervus intermedius. It may include the following:
1.Anterior two thirds of the tongue
2.Soft palate
3.External auditory canal
4.Pinna
.The patient may have associated ipsilateral hearing loss and balance problems.
.A thorough physical examination must be performed, including neuro-otologic and audiometric assessment.
Classic Ramsay Hunt syndrome is ascribed to infection of the geniculate ganglion by herpesvirus 3 (varicella-zoster virus [VZV]).

HISTORY:
*Patients usually present with paroxysmal pain deep within the ear. The pain often radiates outward into the pinna of the ear and may be associated with a more constant, diffuse, and dull background pain.
*The onset of pain usually precedes the rash by several hours and even days.
*Classic Ramsay Hunt syndrome can be associated with the following:
-Vesicular rash of the ear or mouth (as many as 83% of cases),The rash might precede the onset of facial paresis/palsy.
-Ipsilateral lower motor neuron facial paresis/palsy (CN VII)
-Vertigo and ipsilateral hearing loss (CN VII)
-Tinnitus,Otalgia,Headaches,DysarthriaGait,ataxia.
-Fever,Cervical adenopathy.
*Facial weakness usually reaches maximum severity by one week after the onset of symptoms.
*Other cranial neuropathies might be present and may involve cranial nerves (CNs) VIII, IX, X, V, and VI.
*Ipsilateral hearing loss has been reported in as many as 50% of cases.
*Blisters of the skin of the ear canal, auricle, or both may become secondarily infected, causing cellulitis.
EXAMINATION:
.The primary physical findings in classic Ramsay Hunt syndrome include peripheral facial nerve paresis with associated rash or herpetic blisters in the distribution of the nervus intermedius.
.The location of the accompanying rash varies from patient to patient, as does the area innervated by the nervus intermedius. It may include the following:
1.Anterior two thirds of the tongue
2.Soft palate
3.External auditory canal
4.Pinna
.The patient may have associated ipsilateral hearing loss and balance problems.
.A thorough physical examination must be performed, including neuro-otologic and audiometric assessment.
Indirect IA (Inferior Alveolar) nerve block on a model
University of The Pacific Arthur A. Dugoni School of Dentistry present a video illustrating the technique of Inferior Alveolar Nerve Block on a model by Dr. Anders Nattestad, Professor and Director, Department of Oral and Maxillofacial Surgery.
Thursday, 30 December 2010
GOUT PIC
Case of gross hematuria following a game of soccer
A 37 year old male complains of gross hematuria following a game of soccer with his friends at work. He could not recall any particularly severe trauma. On examination both kidneys were enlarged and easy palpable. His blood pressure was raised. A likely diagnosis is :
a) polycystic disease of the kidneys
b) Berger's nephritis
c) systemic lupus erythematosus
d) renal vein thrombosis
e) Goodpasture's syndrome
The correct answer is...................... A
Explanation
In polycystic disease of the kidneys the symptoms or signs first occur between the third and fourth decades of life. These include microscopic and gross hematuria, flank pain and hypertension. The polycystic condition is not confined to the kidneys. Hepatic cysts, usually identified incidentally by sonography, help in making the diagnosis of DPK. These cysts are more likely to be found in adults than in children. Approximately 10% to 40% of patients have berry aneurysms, and approximately 9% of these patients die because of subarachnoid hemorrhages
a) polycystic disease of the kidneys
b) Berger's nephritis
c) systemic lupus erythematosus
d) renal vein thrombosis
e) Goodpasture's syndrome
The correct answer is...................... A
Explanation
In polycystic disease of the kidneys the symptoms or signs first occur between the third and fourth decades of life. These include microscopic and gross hematuria, flank pain and hypertension. The polycystic condition is not confined to the kidneys. Hepatic cysts, usually identified incidentally by sonography, help in making the diagnosis of DPK. These cysts are more likely to be found in adults than in children. Approximately 10% to 40% of patients have berry aneurysms, and approximately 9% of these patients die because of subarachnoid hemorrhages
Mapping the Atrioventricular Node

A 75-year-old woman presented with dyspnea, an awareness of rapid heart action, and permanent atrial fibrillation with a rapid ventricular response that had been resistant to treatment with beta-blockers, calcium-channel blockers, digoxin, and multiple cardioversions. For severe rheumatic aortic and mitral stenosis, she had undergone replacement of the aortic and mitral valves with Starr–Edwards devices in 1970, as seen on chest radiography on admission (Panels A and B, arrows). In 2006, a pacemaker had been implanted for the treatment of bradycardia.
To control the rapid ventricular response to atrial fibrillation, the patient underwent ablation of the atrioventricular node, located just below the aortic valve, where the ablation catheter was positioned (Panel C). Whereas ablation sites are often identified with the use of computerized systems for "electroanatomical mapping," the patient's atrioventricular node was identified on the basis of simple anatomical landmarks, the aortic and mitral valves. The atrioventricular node may be injured by operations or infections because of its proximity to these valves.
After ablation, the patient's condition immediately improved. Atrioventricular-node blocking agents were discontinued, and the only cardiac medications she continued to receive were warfarin and furosemide. Six months after the procedure, the patient remained free of heart-failure symptoms.
Procedures to open obstructed airway
#The tongue is the single most common cause of an airway obstruction. In most cases, the airway can be cleared by simply using the head-tilt/chin-lift technique. This action pulls the tongue away from the air passage in the throat ,See this video:
#The head-tilt/chin-lift is an important procedure in opening the airway; however, use extreme care because excess force in performing this maneuver may cause further spinal injury. In a casualty with a suspected neck injury or severe head trauma, the safest approach to opening the airway is the jaw-thrust technique because in most cases it can be accomplished without extending the neck.See it:
Head tilt chin lift Technique
#The head-tilt/chin-lift is an important procedure in opening the airway; however, use extreme care because excess force in performing this maneuver may cause further spinal injury. In a casualty with a suspected neck injury or severe head trauma, the safest approach to opening the airway is the jaw-thrust technique because in most cases it can be accomplished without extending the neck.See it:
Jaw Thrust Technique
Differences between sutures and fractures in skull x-ray
Linear fracture results from low-energy blunt trauma over a wide surface area of the skull. It runs through the entire thickness of the bone and, by itself, is of little significance except when it runs through a vascular channel, venous sinus groove, or a suture. In these situations, it may cause epidural hematoma, venous sinus thrombosis and occlusion, and sutural diastasis, respectively. Differences between sutures and fractures are summarized in this Table
Click here for enlargment
Algorithm of the cause of Hypokalaemia
A history of vomiting, diarrhoea, or use of medications such as diuretics can be helpful in determining the cause of hypokalaemia. However, in some cases, the cause of hypokalaemia is not readily apparent. In these cases, measurements of BP and urinary potassium excretion, and assessment of acid-base balance are often helpful.

Serum potassium concentrations:
There is no strict correlation between the serum potassium concentration and total body potassium stores. In chronic hypokalaemia, a potassium deficit of 200 to 400 mmol (200 to 400 mEq) is required to lower the serum potassium concentration by 1 mmol/L (1 mEq/L). These estimates are good provided there is no concurrent acid-base abnormality (e.g., for diabetic ketoacidosis or severe non-ketotic hyperglycaemia).
In diabetic ketoacidosis patients may have a normal or even elevated serum potassium concentration at presentation, despite having a marked potassium deficit due to urinary and GI losses.
Spurious hypokalaemia can occur when blood with a high WBC count is left at room temperature due to extraction of potassium by the WBCs. It is therefore important to consider repeating the test for confirmation.


Serum potassium concentrations:
There is no strict correlation between the serum potassium concentration and total body potassium stores. In chronic hypokalaemia, a potassium deficit of 200 to 400 mmol (200 to 400 mEq) is required to lower the serum potassium concentration by 1 mmol/L (1 mEq/L). These estimates are good provided there is no concurrent acid-base abnormality (e.g., for diabetic ketoacidosis or severe non-ketotic hyperglycaemia).
In diabetic ketoacidosis patients may have a normal or even elevated serum potassium concentration at presentation, despite having a marked potassium deficit due to urinary and GI losses.
Spurious hypokalaemia can occur when blood with a high WBC count is left at room temperature due to extraction of potassium by the WBCs. It is therefore important to consider repeating the test for confirmation.

About corneal injuries
Which of the following statements is true regarding corneal injuries?
- A) Patients should have the affected eye patched for 24 hours.
- B) Topical antibiotics are recommended to prevent superinfection.
- C) Foreign bodies should not be removed because of potential further injury to the cornea.
- D) Topical anesthetics should be g...iven to treat the discomfort.
- E) None of the above.
Answer and Discussion
The answer is B.
Controlled studies have not found patching to improve the rate of healing or comfort in patients with traumatic or foreign body abrasions. Patients should be treated with topical antibiotics to prevent superinfection. If a corneal foreign body is detected, an attempt can be made to remove it by irrigation. Topical anesthetics should never be administered or prescribed for pain relief because they delay corneal epithelial healing.
Wednesday, 29 December 2010
Assessment of Head injuries in children
Perform a primary survey and ensure that the child’s airway, cervical spine, breathing and circulation are secure.
Rapidly assess the child’s mental state using the AVPU scale. Use firm supraorbital pressure as the painful stimulus.
* A Alert
* V Responds to voice
* P Responds to pain
----> Purposefully
----> Non-purposefully :
Assess pupil size, equality and reactivity and look for other focal neurological signs.
* Neck and cervical spine – deformity, tenderness, muscle spasm
* Head – scalp bruising, lacerations, swelling, tenderness, bruising behind the ear (Battles sign)
* Eyes – pupil size, equality and reactivity, fundoscopy
* Ears – blood behind the ear drum, CSF leak
* Nose – deformity, swelling, bleeding, CSF leak
* Mouth –dental trauma, soft tissue injuries
* Facial fractures
* Motor function – examine limbs for presence of reflexes and any lateralising weakness
* Perform a formal Glasgow Coma Score
* Consider the possibility of non-accidental injury during secondary survey especially in infants with head injury.
* Other injuries
Rapidly assess the child’s mental state using the AVPU scale. Use firm supraorbital pressure as the painful stimulus.
* A Alert
* V Responds to voice
* P Responds to pain
----> Purposefully
----> Non-purposefully :
- Withdrawal/flexor response
- Extensor response
Assess pupil size, equality and reactivity and look for other focal neurological signs.
Perform a secondary survey looking specifically at:
* Neck and cervical spine – deformity, tenderness, muscle spasm
* Head – scalp bruising, lacerations, swelling, tenderness, bruising behind the ear (Battles sign)
* Eyes – pupil size, equality and reactivity, fundoscopy
* Ears – blood behind the ear drum, CSF leak
* Nose – deformity, swelling, bleeding, CSF leak
* Mouth –dental trauma, soft tissue injuries
* Facial fractures
* Motor function – examine limbs for presence of reflexes and any lateralising weakness
* Perform a formal Glasgow Coma Score
* Consider the possibility of non-accidental injury during secondary survey especially in infants with head injury.
* Other injuries
Photos for Battle's sign
Battle's sign, also called mastoid ecchymosis : consists of bruising over the mastoid process (just behind the auricle), as a result of extravasation of blood along the path of the posterior auricular artery.
It is an indication of fracture of the base of the posterior portion of the skull, and may suggest underlying brain trauma.
Brain herniation Sites
Brain herniation refers to displacement of a portion of the brain from its normal position through openings in the inelastic dura secondary to focal or diffuse intracranial pressure. Recognition of the CT signs of brain herniation on the emergent head CT is critical to proper patient management. The types of brain herniations are schematically illustrated...":a) " Subfalcial (cingulate) herniation ; b) uncal herniation ; c) downward (central, transtentorial) herniation ; d) external herniation ; e) tonsillar herniation.Types a, b, & e are usually caused by focal, ipsilateral space occupying lesions, ie., tumor or axial or extra-axial hemorrhage."
"Schematic representation of various herniation pathways (1) subfalcine, (2) uncal (Transtentorial), (3) cerebellar, and (4) transcalvarium)
OMPHALOCELE PIC


An omphalocele is a birth defect in which the infant's intestine or other abdominal organs stick out of the belly button (navel). In babies with an omphalocele, the intestines are covered only by a thin layer of tissue and can be easily seen.
An omphalocele is a type of hernia. Hernia means "rupture.”
Causes
An omphalocele develops as a baby grows inside the mother's womb. The muscles in the abdominal wall (umbilical ring) do not close properly. As a result, the intestine remains outside the umbilical cord.
Approximately 25 - 40% of infants with an omphalocele have other birth defects. They may include genetic problems (chromosomal abnormalities), congenital diaphragmatic hernia, and heart defects.an example is Beckwith-Wiedemann syndrome.
Treatment
Omphaloceles are repaired with surgery, although not always immediately. A sac protects the abdominal contents and allows time for other more serious problems (such as heart defects) to be dealt with first, if necessary.
To fix an omphalocele, the sac is covered with a special man-made material, which is then stitched in place. Slowly, over time, the abdominal contents are pushed into the abdomen.
When the omphalocele can comfortably fit within the abdominal cavity, the man-made material is removed and the abdomen is closed.
Sometimes the omphalocele is so large that it cannot be placed back inside the infant's abdomen. The skin around the omphalocele grows and eventually covers the omphalocele. The abdominal muscles and skin can be repaired when the child is older to achieve a better cosmetic outcome.
Delivery Room Management of the Newborn omphalocele
Medical students song :D :D
A very funny song for all medical and nursing students! Its about our lives...
Benign Prostatic Hyperplasia
Many men with benign prostatic hyperplasia experience urinary problems related to the condition. As the prostate enlarges, the gland places increasing pressure on the urethra, often resulting in difficulty beginning or ending urination, an inability to completely empty the bladder, decreased urine flow, and frequent urination. In the most severe cases, complete blockage of the urethra occurs, which may lead to kidney damage.
From microscopyu.com
From microscopyu.com
Benign Prostatic Hyperplasia at 20x Magnification :
Part of the male reproductive system, the prostate gland produces and stores seminal fluids, releasing them into the urethra when semen emission occurs. The gland is located directly below the bladder and surrounds the upper part of the urethra. During adolescence the gland usually matures and reaches a size comparable to that of a walnut. The dimensions of the gland generally remain unchanged for several decades, but in most older men, the prostate begins to enlarge as the size of its cells increases, a process commonly referred to as benign prostatic hyperplasia (BPH) or hypertrophy. According to recent estimates, more than 50 percent of men between the ages of 50 and 60 experience benign prostatic hyperplasia, and over 90 percent of those 70 to 90 years old have developed the condition. Researchers do not yet completely understand the cause of this physiological change, but it is widely thought that elevated levels of the female sex hormone estradiol and increased manufacture of dihydrotestosterone, a derivative of the male sex hormone testosterone, contribute to the condition.Benign Prostatic Hyperplasia at 4x Magnification :
Men with only mild symptoms of benign prostatic hyperplasia may elect not to undergo any treatment or to simply take a wait-and-see attitude, visiting the doctor regularly for monitoring until signs suggest a more active approach is needed. For those who seek treatment, a number of options are available. For example, drugs such as alpha blockers and finasteride may be used alone or in conjunction with one another to relax prostatic smooth muscle and decrease the size of the prostate gland. Individuals that are not responsive to the typical medications, however, may require a more invasive form of treatment, such as balloon dilation of the urethra or any of several different surgical techniques, including transurethral incision of the prostate (TUIP), transurethral resection of the prostate (TURP), or open prostatectomy. The various treatments for benign prostatic hyperplasia are associated with a number of risks and side effects, which can include serious conditions like incontinence and impotence.
Tuesday, 28 December 2010
Ambulation Algorithm

FOOTNOTES:
1. Non-weight bearing: Patient is unable to bear weight through both lower extremities or weight-bearing through both lower extremities is contraindicated.
2. Partial weight bearing: This will include situations where the patient may be allowed: a) Limited weight bearing on one lower extremity and full weight bearing on the other extremity; b) Partial weight bearing through both lower extremities.
3. Safety risks may include: decreased cognition; decreased ability to cooperate/ combativeness; medical stability.
4. Factors that contribute to low safety risk: a) Lack of combativeness; b) Ability to follow commands; c) Medical stability; d) Experience with the assistive device.
5. Factors that contribute to high safety risk: a) Combativeness; b) Lack of ability to follow commands; c) Medical instability; d) Lack of experience with
the assistive device, e) neurological deficits.
Anterior Sternal Dislocation
An 83-year-old man was admitted to the acute medical ward after having fallen down in his home. On admission he was confused and agitated.
Physical examination revealed a swelling with bruising over his right sternoclavicular joint (Panel A) and periorbital bruising. He had a white-cell count of 14×103 per cubic millimeter, a C-reactive protein level of 56 mg per liter, and a urinalysis that was positive for a urinary tract infection. A social history was taken and revealed no suggestion of abuse. Radiography of the chest (Panel B) showed a right sternoclavicular dislocation, which was clinically confirmed to be anterior.
Anterior sternoclavicular dislocations often result from an indirect force to the shoulder, rotating the shoulder posteriorly. The physician must always consider the possibility of abuse having caused this type of injury. The patient was treated for his urinary tract infection. His anterior sternoclavicular dislocation was treated conservatively. The confusion resolved, and after a short period of rehabilitation, he regained good function of his right upper limb.
Physical examination revealed a swelling with bruising over his right sternoclavicular joint (Panel A) and periorbital bruising. He had a white-cell count of 14×103 per cubic millimeter, a C-reactive protein level of 56 mg per liter, and a urinalysis that was positive for a urinary tract infection. A social history was taken and revealed no suggestion of abuse. Radiography of the chest (Panel B) showed a right sternoclavicular dislocation, which was clinically confirmed to be anterior.
Anterior sternoclavicular dislocations often result from an indirect force to the shoulder, rotating the shoulder posteriorly. The physician must always consider the possibility of abuse having caused this type of injury. The patient was treated for his urinary tract infection. His anterior sternoclavicular dislocation was treated conservatively. The confusion resolved, and after a short period of rehabilitation, he regained good function of his right upper limb.
IDENTIFICATION of Giardia lamblia
Giardiasis is diagnosed by finding cysts or trophozoites in the feces, and both life cycle stages have a characteristic appearance.
The trophozoites average 10-20 μm in length, 5-15 μm in width, have a distinct “teardrop” or “pear” shape and two nuclei at the anterior end . The two nuclei, laterally located in the bilaterally symmetrical trophozoite, have central karysomes present; nuclei are not visible in unstained preparations.
Four pairs of flagella arise from basal bodies clustered between the two nuclei. The broad anterior end of the trophozoite contains a concave area which covers half the ventral surface. This is the adhesive or sucking disc that allows the parasite to attach to the mucosa of the patient’s small intestine. When viewed from the side G. lamblia is spoon shaped.
Microscopists often say that G. lamblia trophozoites are "staring back at them and smiling." The trophozoites also contain an axostyle (consisting of two axonemes) or dark transverse rod, which may be a supportive element. Two curved median or parabasal bodies cross the axoneme at an oblique angle giving the parasite its “smile”.
The cysts average 8-19 μm in length, 7-10 μm in width, are typically oval, but also ellipsoidal, or round and contain 4 nuclei and remnants of the axostyle. The 4 nuclei are usually located on one end; there is no peripheral chromatin and the karyosomes are smaller than in the trophozoites. Staining may cause shrinkage making the cytoplasm pull away from the cyst wall. Many fibrils (flagellar remnants) and median bodies may be seen in the cytoplasm. Because of these unique characteristics, when found, G. lamblia is one of the easiest intestinal protozoans of humans to identify.
 |
| Giardia lamblia - trophozoite 10-20 µm long by 5-15 µm wide 1. Note sucking disk. 2. Iron-hematoxylin stain |
The trophozoites average 10-20 μm in length, 5-15 μm in width, have a distinct “teardrop” or “pear” shape and two nuclei at the anterior end . The two nuclei, laterally located in the bilaterally symmetrical trophozoite, have central karysomes present; nuclei are not visible in unstained preparations.
Four pairs of flagella arise from basal bodies clustered between the two nuclei. The broad anterior end of the trophozoite contains a concave area which covers half the ventral surface. This is the adhesive or sucking disc that allows the parasite to attach to the mucosa of the patient’s small intestine. When viewed from the side G. lamblia is spoon shaped.
Microscopists often say that G. lamblia trophozoites are "staring back at them and smiling." The trophozoites also contain an axostyle (consisting of two axonemes) or dark transverse rod, which may be a supportive element. Two curved median or parabasal bodies cross the axoneme at an oblique angle giving the parasite its “smile”.
The cysts average 8-19 μm in length, 7-10 μm in width, are typically oval, but also ellipsoidal, or round and contain 4 nuclei and remnants of the axostyle. The 4 nuclei are usually located on one end; there is no peripheral chromatin and the karyosomes are smaller than in the trophozoites. Staining may cause shrinkage making the cytoplasm pull away from the cyst wall. Many fibrils (flagellar remnants) and median bodies may be seen in the cytoplasm. Because of these unique characteristics, when found, G. lamblia is one of the easiest intestinal protozoans of humans to identify.
 |
| Giardia lamblia cysts 8-19 µm long by 7-10 µm wide |
Pinna Contusion and Hematoma
Blunt external ear trauma may cause a contusion or hematoma of the pinna which, if untreated, may result in cartilage necrosis and chronic scarring or further cartilage formation and permanent deformity or "cauliflower ear." Open injuries include lacerations (with and without cartilage exposure) and avulsions.
Pinna Contusion. Contusion without hematoma is present. Reevaluation in 24 hours is recommended to ensure a drainable hematoma has not formed.
Pinna Hematoma. A hematoma has developed, characterized by swelling, discoloration, ecchymosis, and fluctuance. Immediate incision and drainage or aspiration is indicated, followed by an ear compression dressing.
Pinna Contusion. Contusion without hematoma is present. Reevaluation in 24 hours is recommended to ensure a drainable hematoma has not formed.
Pinna Hematoma. A hematoma has developed, characterized by swelling, discoloration, ecchymosis, and fluctuance. Immediate incision and drainage or aspiration is indicated, followed by an ear compression dressing.
Monday, 27 December 2010
Complications of Sickle cell disease
Medical mnemonic for the Sickle cell disease complications
Strokes/ Swelling of hands and feet/ Spleen problems
Infections/ Infarctions
Crises (painful, sequestration, aplastic)/ Cholelithiasis/ Chest syndrome/ Chronic hemolysis/ Cardiac problems
Kidney disease
Liver disease/ Lung problems
Erection (priapism)/ Eye problems (retinopathy)
SICKLE:
Strokes/ Swelling of hands and feet/ Spleen problems
Infections/ Infarctions
Crises (painful, sequestration, aplastic)/ Cholelithiasis/ Chest syndrome/ Chronic hemolysis/ Cardiac problems
Kidney disease
Liver disease/ Lung problems
Erection (priapism)/ Eye problems (retinopathy)
Blue Tongue Disease !!!
No, this child does not have Blue Tongue Disease! (There is no such thing--in humans anyways. Such a disease does exist, but it only affects cattle, goats, sheep and deer.) A few drops of blue food coloring were applied to demonstrate the general size and location of the (otherwise pink) fungiform papillae which are the little bumps scattered all over the top surface of the tongue. They are usually difficult to see unless an overgrowth of filiform papillae causes the ordinarily pink velvet of the tongue to turn white, in which case the fungiform papillae stand out as red dots.
Layers of the Abdominal Wall with Function
The layers of the abdominal wall vary, depending on where it is you are looking.
At the lateral side of the abdomen there is a dotted line passing through the abdominal wall. Note the layers must pass through to get to the peritoneal cavity:
1. skin
2. superficial fascia (this may be as thin as or less than a half inch or as thick as 6 inches or more)
3. deep fascia (all skeletal muscle is surrounded within its own deep fascia). The deep fascia of the abdominal wall is different than that found around muscles of the extremities, however. It is of the loose connective tissue variety. It is necessary in the abdominal wall because it offers more flexibility for a variety of functions of the abdomen. At certain points, this fascia may become aponeurotic and serve as attachments for the muscle to bone or to each other, as is the case at the linea alba.
4. subserous fascia also known at extraperitoneal fascia (a layer of loose connective tissue that serves as a glue to hold the peritoneum to the deep fascia of the abdominal wall or to the outer lining of the GI tract. It may receive different names depending on its location (i.e. transversalis fascia when it is deep to that muscle, psoas fascia when it is next to that muscles, iliac fascia, etc.)
5. peritoneum (a thin one cell thick membrane that lines the abdominal cavity and in certain places reflects inward to form a double layer of peritoneum) Double layers of peritoneum are called mesenteries, omenta, falciform ligaments, lienorenal ligament, etc.)
--At the anterior wall of the abdomen, in the midline there is no muscle.
--If we look at the wall inferior to the level of the belly button (umbilicus), you will see that the superficial fascia has become divided into 2 parts:
* a superficial fatty part that is continuous with the same layer over the rest of the body (Camper's fascia)
* a deep membranous layer that is continuous down into the perineum to surround the penis and to form a layer of the scrotum. (Scarpa's fascia)
At the lateral side of the abdomen there is a dotted line passing through the abdominal wall. Note the layers must pass through to get to the peritoneal cavity:
1. skin
2. superficial fascia (this may be as thin as or less than a half inch or as thick as 6 inches or more)
3. deep fascia (all skeletal muscle is surrounded within its own deep fascia). The deep fascia of the abdominal wall is different than that found around muscles of the extremities, however. It is of the loose connective tissue variety. It is necessary in the abdominal wall because it offers more flexibility for a variety of functions of the abdomen. At certain points, this fascia may become aponeurotic and serve as attachments for the muscle to bone or to each other, as is the case at the linea alba.
4. subserous fascia also known at extraperitoneal fascia (a layer of loose connective tissue that serves as a glue to hold the peritoneum to the deep fascia of the abdominal wall or to the outer lining of the GI tract. It may receive different names depending on its location (i.e. transversalis fascia when it is deep to that muscle, psoas fascia when it is next to that muscles, iliac fascia, etc.)
5. peritoneum (a thin one cell thick membrane that lines the abdominal cavity and in certain places reflects inward to form a double layer of peritoneum) Double layers of peritoneum are called mesenteries, omenta, falciform ligaments, lienorenal ligament, etc.)
--At the anterior wall of the abdomen, in the midline there is no muscle.
--If we look at the wall inferior to the level of the belly button (umbilicus), you will see that the superficial fascia has become divided into 2 parts:
* a superficial fatty part that is continuous with the same layer over the rest of the body (Camper's fascia)
* a deep membranous layer that is continuous down into the perineum to surround the penis and to form a layer of the scrotum. (Scarpa's fascia)
Lap dermoid cystectomy
a large size glove can be used as an endobag as is shown in this case of lap dermoid cystectomy.careful dissection.of the dermoid,enclosing it in a glove/endobag and removal are the features of this case.
Sunday, 26 December 2010
The lady between two majors

Bicipital groove: attachments of muscles near it
"The lady between two majors"
Teres major attaches to medial lip of groove.
Pectoralis major to lateral lip of groove.
Latissimus (Lady) is on floor of groove, between the 2 majors.
Pectoralis major to lateral lip of groove.
Latissimus (Lady) is on floor of groove, between the 2 majors.
Myocardial ischemia in older patients
Which of the following symptoms is more likely to represent myocardial ischemia in older patients?
The answer is B.
Exertional angina (chest pain) is the most common manifestation of myocardial ischemia in young and middle-age persons. Because of their more sedentary lifestyle or possibly a difference in pathophysiology, this may not be true in elderly patients. Instead of exertional chest pain, ischemia may be more commonly manifested as dyspnea in elderly patients. Other elderly patients with CAD may be completely asymptomatic, although silent ischemia may be demonstrated by stress testing or Holter monitoring.
- A) Chest pain
- B) Dyspnea
- C) Diaphoresis
- D) Back pain
- E) Jaw pain
Answer and Discussion
The answer is B.
Exertional angina (chest pain) is the most common manifestation of myocardial ischemia in young and middle-age persons. Because of their more sedentary lifestyle or possibly a difference in pathophysiology, this may not be true in elderly patients. Instead of exertional chest pain, ischemia may be more commonly manifested as dyspnea in elderly patients. Other elderly patients with CAD may be completely asymptomatic, although silent ischemia may be demonstrated by stress testing or Holter monitoring.
Note:
Instead of exertional chest pain, ischemia may be more commonly manifested as dyspnea in elderly patients.
Synthesis of eicosanoid autacoids
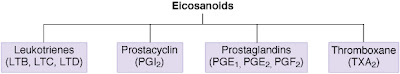
The eicosanoids are an important group of endogenous fatty acid derivatives that are produced from arachidonic acid, a 20-carbon fatty acid lipid in cell membranes. Major families of eicosanoids include the straight-chain derivatives (leukotrienes) and cyclic derivatives (prostacyclin, prostaglandins, and thromboxane). Inhibitors of the eicosanoids are shown in Figure below.
Diagram of meniscal tear patterns
Meniscal injuries can be classified according to their tear patterns. A vertical or longitudinal tear occurs in line with the circumferential fibers of the meniscus . If long enough, this tear is known as a bucket-handle tear. At arthroscopy, the bucket-handle tear may be seen as being attached anteriorly and posteriorly. Alternatively, it may be detached at either end or transected in the middle with unstable anterior and posterior flaps. A bucket-handle tear may displace into the intercondylar notch, where it may cause true locking of the knee joint.
-Oblique tears are also known as flap or parrot beak tears and are perhaps the most common . These occur generally at the junction of the posterior and middle thirds.
-Radial tears occur in a similar location. They extend from the inner free margin toward the periphery . If such a tear reaches the periphery, it transects the meniscus and renders the hoop stress-distributing capacities of the meniscus useless. Such a tear is the functional equivalent of a total meniscectomy.
-Horizontal cleavage tears usually occur in older individuals. They extend from the inner free margin peripherally to the intrameniscal substance where myxoid degeneration may be present. These tears divide the meniscus into superior and inferior flaps, either of which may be unstable
-Complex degenerative tears occur in older patients. Osteoarthritic changes may be visible on plain radiographs, and chondromalacia of the articular surfaces is commonly encountered. The tears occur in multiple planes .
(A) Vertical or longitudinal (Bucket-handle), (B) Flap or Oblique, (C) Radial or Transverse, (D) Horizontal, (E) Complex degenerative.
-Oblique tears are also known as flap or parrot beak tears and are perhaps the most common . These occur generally at the junction of the posterior and middle thirds.
-Radial tears occur in a similar location. They extend from the inner free margin toward the periphery . If such a tear reaches the periphery, it transects the meniscus and renders the hoop stress-distributing capacities of the meniscus useless. Such a tear is the functional equivalent of a total meniscectomy.
-Horizontal cleavage tears usually occur in older individuals. They extend from the inner free margin peripherally to the intrameniscal substance where myxoid degeneration may be present. These tears divide the meniscus into superior and inferior flaps, either of which may be unstable
-Complex degenerative tears occur in older patients. Osteoarthritic changes may be visible on plain radiographs, and chondromalacia of the articular surfaces is commonly encountered. The tears occur in multiple planes .
Nutcracker phenomenon
It results most commonly from the compression of the left renal vein between the abdominal aorta (AA) and superior mesenteric artery (SMA), although other variants exist. The name derives from the fact that, in the sagittal view, the SMA and AA (with some imagination) appear to be a nutcracker crushing a nut (the renal vein).
There is a wide spectrum of clinical presentations and diagnostic criteria are not well defined resulting in frequently delayed or incorrect diagnosis. This condition is not to be confused with superior mesenteric artery syndrome, which is the compression of the third portion of the duodenum by the SMA and the AA.
This Computed tomography for a 52-year-old woman with mild episodic gross hematuria revealed compression of the left renal vein between the superior mesenteric artery (SMA) and the aorta (Ao) before the vein merges into the inferior vena cava (IVC). This compression caused marked dilatation of the distal part of the renal vein (RV). The renal venous congestion caused hematuria, presumably through the rupture of submucosal veins into the renal pelvis. No treatment was given. Entrapment of the renal vein is a known cause of hematuria.
There is a wide spectrum of clinical presentations and diagnostic criteria are not well defined resulting in frequently delayed or incorrect diagnosis. This condition is not to be confused with superior mesenteric artery syndrome, which is the compression of the third portion of the duodenum by the SMA and the AA.
This Computed tomography for a 52-year-old woman with mild episodic gross hematuria revealed compression of the left renal vein between the superior mesenteric artery (SMA) and the aorta (Ao) before the vein merges into the inferior vena cava (IVC). This compression caused marked dilatation of the distal part of the renal vein (RV). The renal venous congestion caused hematuria, presumably through the rupture of submucosal veins into the renal pelvis. No treatment was given. Entrapment of the renal vein is a known cause of hematuria.
Saturday, 25 December 2010
lymphoid organs (Organs of the Immune System)
The organs of the immune system are positioned throughout the body. They are called lymphoid organs because they are home to lymphocytes, small white blood cells that are the key players in the immune system.
Bone marrow, the soft tissue in the hollow center of bones, is the ultimate source of all blood cells, including white blood cells destined to become immune cells. The thymus is an organ that lies behind the breastbone; lymphocytes known as T lymphocytes, or just "T cells," mature in the thymus.
Lymphocytes can travel throughout the body using the blood vessels. The cells can also travel through a system of lymphatic vessels that closely parallels the body’s veins and arteries. Cells and fluids are exchanged between blood and lymphatic vessels, enabling the lymphatic system to monitor the body for invading microbes. The lymphatic vessels carry lymph, a clear fluid that bathes the body’s tissues.
Small, bean-shaped lymph nodes are laced along the lymphatic vessels, with clusters in the neck, armpits, abdomen, and groin. Each lymph node contains specialized compartments where immune cells congregate, and where they can encounter antigens.
Immune cells and foreign particles enter the lymph nodes via incoming lymphatic vessels or the lymph nodes' tiny blood vessels. All lymphocytes exit lymph nodes through outgoing lymphatic vessels. Once in the bloodstream, they are transported to tissues throughout the body. They patrol everywhere for foreign antigens, then gradually drift back into the lymphatic system, to begin the cycle all over again.
The spleen is a flattened organ at the upper left of the abdomen. Like the lymph nodes, the spleen contains specialized compartments where immune cells gather and work, and serves as a meeting ground where immune defenses confront antigens.
Bone marrow, the soft tissue in the hollow center of bones, is the ultimate source of all blood cells, including white blood cells destined to become immune cells. The thymus is an organ that lies behind the breastbone; lymphocytes known as T lymphocytes, or just "T cells," mature in the thymus.
Lymphocytes can travel throughout the body using the blood vessels. The cells can also travel through a system of lymphatic vessels that closely parallels the body’s veins and arteries. Cells and fluids are exchanged between blood and lymphatic vessels, enabling the lymphatic system to monitor the body for invading microbes. The lymphatic vessels carry lymph, a clear fluid that bathes the body’s tissues.
Small, bean-shaped lymph nodes are laced along the lymphatic vessels, with clusters in the neck, armpits, abdomen, and groin. Each lymph node contains specialized compartments where immune cells congregate, and where they can encounter antigens.
Immune cells and foreign particles enter the lymph nodes via incoming lymphatic vessels or the lymph nodes' tiny blood vessels. All lymphocytes exit lymph nodes through outgoing lymphatic vessels. Once in the bloodstream, they are transported to tissues throughout the body. They patrol everywhere for foreign antigens, then gradually drift back into the lymphatic system, to begin the cycle all over again.
The spleen is a flattened organ at the upper left of the abdomen. Like the lymph nodes, the spleen contains specialized compartments where immune cells gather and work, and serves as a meeting ground where immune defenses confront antigens.
Classification of inflammatory arthritis
Inflammatory arthritis is generally classified into seropositive and seronegative groups. These are based on the presence of rheumatoid factor, an immunoglobulin which reacts with gamma globulin, in the blood of the majority of patients with seropositive disease and in a small minority of patients with seronegative disease. The prototype seropositive form of arthritis is rheumatoid arthritis. Other members include the group of conditions labelled collagen vascular diseases, such as systemic lupus erythematosus, scleroderma, vasculitis, Sjogren’s syndrome. Only rheumatoid arthritis will be considered in this paper.
Among the seronegative inflammatory joint diseases is a group labelled spondyloarthritis. This condition is characterized by inflammatory disease of the joints of the back, both the sacroiliac joints and the apophyseal joints of the spine. Members of this group include ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and arthritis of inflammatory bowel disease. While the prototype for this group is ankylosing spondylitis, psoriatic arthritis will also be discussed.
In addition to the presence of rheumatoid factor, there are extra-articular features which distinguish the seropositive from the seronegative forms of inflammatory arthritis.
Among the seronegative inflammatory joint diseases is a group labelled spondyloarthritis. This condition is characterized by inflammatory disease of the joints of the back, both the sacroiliac joints and the apophyseal joints of the spine. Members of this group include ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and arthritis of inflammatory bowel disease. While the prototype for this group is ankylosing spondylitis, psoriatic arthritis will also be discussed.
In addition to the presence of rheumatoid factor, there are extra-articular features which distinguish the seropositive from the seronegative forms of inflammatory arthritis.
A case of Inflammatory Arthritis
A 34 year old male has a long history of several subacute attacks of self-limited inflammatory arthritis. Crystals have been retrieved from a joint aspirate. Radiography of his knee is likely to demonstrate:
a) subperiosteal thickening
b) marginal articular erosions
c) central articular erosions
d) chondrocalcinosis
e) subchondral bony sclerosis
The correct answer is D
Explanation
Chondrocalcinosis is simply the term for the finding of radio-opaque crystals in hyaline or fibrocartilage. These salts may consist of calcium pyrophosphate dihydrate, dicalcium phosphate dihydrate or hydroxyapatite. Crystals may also be deposited in bursae, capsules, ligaments and tendons.
Chondrocalcinosis may accompany a variety of diseases, but is not a disease entity merely a physical sign thereof. Used properly, the term pseudogout refers to the clinical syndrome of one or more acute or subacute attacks of self-limited inflammatory arthritis caused by crystal-induced synovitis, proven by recovery of the crystals from a joint aspirate. Most people with chondrocalcinosis never have a single acute episode of pseudogout.
CPPD crystal deposition disease is the general term that encompasses chondrocalcinosis, pseudogout, a distinctive arthropathy and a host of variations. During acute attacks (pseudogout) of crystal-induced synovitis, the usual radiological findings are soft-tissue oedema and joint effusion. Chondrocalcinosis may or may not be present. The cartilage and articular bone are often normal. The chronic arthropathy is more distinctive. It is most frequent in the patellofemoral, radiocarpal metacarpophalangeal and elbow joints.
Although the findings superficially resemble osteoarthritis, there are several important differences beyond the unique distribution. The arthropathy is characterized by cartilage loss, multiple subchondral cystic rarefactions, structural collapse of the articular surface, and the presence of many small intra-articular fragments, all without much bone sclerosis. In addition to the usual target sites, these changes may be observed in the hips, knees and sacroiliac joints. Chondrocalcinosis, which does not have to accompany the arthropathy, is seen most commonly in the large joints such as the knee, hip and shoulder as well as the symphysis pubis.
a) subperiosteal thickening
b) marginal articular erosions
c) central articular erosions
d) chondrocalcinosis
e) subchondral bony sclerosis
The correct answer is D
Explanation
Chondrocalcinosis is simply the term for the finding of radio-opaque crystals in hyaline or fibrocartilage. These salts may consist of calcium pyrophosphate dihydrate, dicalcium phosphate dihydrate or hydroxyapatite. Crystals may also be deposited in bursae, capsules, ligaments and tendons.
Chondrocalcinosis may accompany a variety of diseases, but is not a disease entity merely a physical sign thereof. Used properly, the term pseudogout refers to the clinical syndrome of one or more acute or subacute attacks of self-limited inflammatory arthritis caused by crystal-induced synovitis, proven by recovery of the crystals from a joint aspirate. Most people with chondrocalcinosis never have a single acute episode of pseudogout.
CPPD crystal deposition disease is the general term that encompasses chondrocalcinosis, pseudogout, a distinctive arthropathy and a host of variations. During acute attacks (pseudogout) of crystal-induced synovitis, the usual radiological findings are soft-tissue oedema and joint effusion. Chondrocalcinosis may or may not be present. The cartilage and articular bone are often normal. The chronic arthropathy is more distinctive. It is most frequent in the patellofemoral, radiocarpal metacarpophalangeal and elbow joints.
Although the findings superficially resemble osteoarthritis, there are several important differences beyond the unique distribution. The arthropathy is characterized by cartilage loss, multiple subchondral cystic rarefactions, structural collapse of the articular surface, and the presence of many small intra-articular fragments, all without much bone sclerosis. In addition to the usual target sites, these changes may be observed in the hips, knees and sacroiliac joints. Chondrocalcinosis, which does not have to accompany the arthropathy, is seen most commonly in the large joints such as the knee, hip and shoulder as well as the symphysis pubis.
Testicular microliths in a new born
The above ulltrasound images and Color Doppler image show testicular microliths (left testis) in a new born baby.
Testicular calcifications can occur in any age group; however the occurrence of this condition in a newborn is very rare. The color Doppler study showed normal vascularity in the affected testis.
Such cases need to be followed up for changes such as germ cell tumor and more benign conditions such as epididymitis, orchitis and varicocele as well as testicular atrophy. Studies show possible link between Testicular microlithiasis in infants and Down's syndrome.
Friday, 24 December 2010
Keloids of the Auricle
Keloid formation of the auricle's ear lobe is a rare complication of ear ring use. It occurs more commonly in African Americans than Caucasians. Treatments is surgical excision followed by repeated steroid injections.
Estrogen as an initial treatment for symptomatic labial adhesions
The initial treatment of choice for symptomatic labial adhesions is :
A) testosterone cream
B) estrogen cream
C) GnRH antagonist
D) hydrocortisone cream
E) surgical separation
The answer is: ( B ).
Labial adhesions are common in prepubertal females. The cause is thought related to low levels of circulating estrogen. Most women with small areas of labial adhesions are asymptomatic. However, interference with urination or accumulation of urine behind the adhesion can lead to discomfort and symptoms. Dysuria and recurrent vulvar and vaginal infections are associated symptoms. In rare situations urinary retention may occur. Asymptomatic labial fusion usually does not require treatment. Symptomatic adhesions may be treated with a short course of estrogen cream applied twice daily for 7 to 10 days; this may separate the labia.
A new alternative treatment is to use estrogen transdermal patches in close proximity to the labia. When medical treatment fails or if severe urinary symptoms exist, surgical separation of the labia is indicated. This can be done as an office procedure using 1% to 2% topical xylocaine gel. Because of inadequate levels of estrogen, recurrences of labial adhesion are common until puberty. Following puberty, the condition usually resolves spontaneously. Improved hygiene and removal of vulvar irritants may help prevent recurrences.
A) testosterone cream
B) estrogen cream
C) GnRH antagonist
D) hydrocortisone cream
E) surgical separation
Answer and Discussion
The answer is: ( B ).
Labial adhesions are common in prepubertal females. The cause is thought related to low levels of circulating estrogen. Most women with small areas of labial adhesions are asymptomatic. However, interference with urination or accumulation of urine behind the adhesion can lead to discomfort and symptoms. Dysuria and recurrent vulvar and vaginal infections are associated symptoms. In rare situations urinary retention may occur. Asymptomatic labial fusion usually does not require treatment. Symptomatic adhesions may be treated with a short course of estrogen cream applied twice daily for 7 to 10 days; this may separate the labia.
A new alternative treatment is to use estrogen transdermal patches in close proximity to the labia. When medical treatment fails or if severe urinary symptoms exist, surgical separation of the labia is indicated. This can be done as an office procedure using 1% to 2% topical xylocaine gel. Because of inadequate levels of estrogen, recurrences of labial adhesion are common until puberty. Following puberty, the condition usually resolves spontaneously. Improved hygiene and removal of vulvar irritants may help prevent recurrences.
Actinic Keratosis of Scalp

This photo shows An actinic keratosis of the scalp. These lesions are often difficult to see.
Description:
ABCD causes of BUN:creatinine elevation
BUN stands for blood urea nitrogen which measures the amount of urea nitrogen, a waste product of protein metabolism, in the blood. Urea is formed by the liver and carried by the blood to the kidneys for excretion. Because urea is cleared from the bloodstream by the kidneys, a test measuring how much urea nitrogen remains in the blood can be used as a test of renal function. However, there are many factors besides renal disease that can cause BUN alterations, including protein breakdown, hydration status, and liver failure.

values for BUN:
* Adult: 7-20 mg/100 ml; men may have slightly higher values than women
* Pregnancy: values decrease about 25%
* Newborn: values slightly lower than adult ranges
* Elderly: values may be slightly increased due to lack of renal concentration
##BUN:creatinine elevation: causes ABCD:

values for BUN:
* Adult: 7-20 mg/100 ml; men may have slightly higher values than women
* Pregnancy: values decrease about 25%
* Newborn: values slightly lower than adult ranges
* Elderly: values may be slightly increased due to lack of renal concentration
##BUN:creatinine elevation: causes ABCD:
- Azotremia (pre-renal)
- Bleeding (GI)
- Catabolic status
- Diet (high protein parenteral nutrition)
Cranial Nerve 9 Dysfunction Pic
Thursday, 23 December 2010
Osteoporosis of aging (senile or postmenopausal osteoporosis)
Most common form of generalized osteoporosis. As a person ages, the bones lose density and become more brittle, fracturing more easily and healing more slowly. Many elderly persons are also less active and have poor diets that are deficient in protein. Females are affected more often and more severely than males, as postmenopausal women have deficient gonadal hormone levels and decreased osteoblastic activity.
Osteoporosis of aging. Generalized demineralization of the spine in a postmenopausal woman. The cortex appears as a thin line that is relatively dense and prominent (picture-frame pattern).
Osteoporosis of aging. Generalized demineralization of the spine in a postmenopausal woman. The cortex appears as a thin line that is relatively dense and prominent (picture-frame pattern).
Toxoplasmosis in Immune-Suppressed Patients
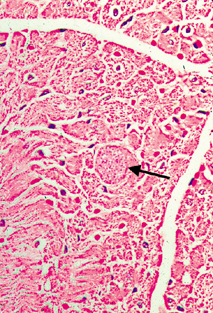
Toxoplasma encephalitis (inflammation of the brain) and Toxoplasma myocarditis (inflammation of the heart) are well recognised opportunistic infections in patients who are immune suppressed, particularly in relation to AIDS and chemotherapy for cancer. The Toxoplasma encephalitis has the usual appearance of an encephalitis from any cause, that is, focal areas of death of cerebral tissue associated with a mononuclear inflammatory cell infiltrate. But in addition, Toxoplasma cysts are found in the affected brain tissue.
This figures are from the heart of a middle aged male who died from AIDS. The Toxoplasma cyst is expanding the myocardial muscle fibre. In this case there is no inflammatory reaction associated with the cyst. The presence of an inflammatory reaction is variable.
This figures are from the heart of a middle aged male who died from AIDS. The Toxoplasma cyst is expanding the myocardial muscle fibre. In this case there is no inflammatory reaction associated with the cyst. The presence of an inflammatory reaction is variable.
Subscribe to:
Posts (Atom)